September 30, 2016.
By Sophie Lewis
[infogram id=”76287f2e-ef27-4c88-a95d-05e87ca89aee”]Four million Australians living in low income households and 2.6 million living in rural areas, are paying the price for poor health.
The latest National Health Survey by the Australian Bureau of Statistics found the obesity epidemic has affected the most marginalised, by pay check and postcode.
Manager of Population Health at Merri Community Health Services, Maryanne Tadic, maintained there is a definite link between socioeconomic disadvantage and weight status in Australia, reflecting a growing gulf between rich and poor.
“There is profound evidence that says the more well off you are, the better health you have,” she said.
This health gradient has appeared globally and particularly in Australia; a slope that has continued to rise.
Not only does the ill-health of the have-nots guarantee a risk of overweight and obesity, but has the propensity for long-term chronic diseases, such as type 2 diabetes and heart disease.
“People who are experiencing socioeconomic disadvantage don’t have the privilege of choice around food or purchasing food, where they live and the hours they work; influencing their social connectedness and overall health,” Tadic said.
“The inability to afford healthy food, or live in a place that is well-connected to make healthy decisions is a significant determinant of overweight and obesity.”
Food security – one’s access and availability to nutritious food – has become a concern in Australia, with around four per cent of the population living in food-insecure households.
This has emerged as paradox: those suffering from food insecurity were more likely to be overweight and obese – the biggest members of society, with the least.
Tadic pinpointed Fawkner in Northern Melbourne as a suburb of high socioeconomic disadvantage, with issues of food insecurity.
Merri Health has assisted the community of Fawkner through projects such as the ‘Community Grocer’ to address food insecurity.
Proportionally, health inequality was found to be most prevalent in women.
In 2015, a significantly larger proportion of women living in areas of disadvantage were overweight or obese (61.1%), than women living in areas of the least disadvantage (47.8%) – a pattern not apparent in men.
[infogram id=”60872e3a-f9c5-456b-88a9-a9b0eaf3219c”]This disparity was even larger in Victoria, where the risk of obesity was 20-40% higher in women who have low incomes and were experiencing food insecurity.
Tadic said transport and location gravely impact a woman’s diet in socioeconomically disadvantaged communities.
“When looking at a lower-socioeconomic, isolated suburb like Fawkner, it is much easier to get a take away meal than it is to get good quality fruit and vegetables. Ultimately the unhealthy decision is the easiest decision.”
A disparity in geographical location and health also mirror this trend.
[infogram id=”7556f530-68b3-4b15-bfa6-7a14d88f162c”]In the outer regional and remote areas of Lodden, Mallee and the Murray in Victoria, 41% of adults were obese in comparison with 16% in Melbourne’s Inner East suburbs.
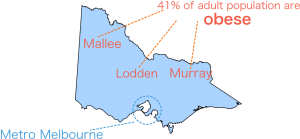
A correlation appears most dramatically in women, where the rate of obesity was 12% higher in outer regional and remote women, when compared with those living in major cities.
A HESSE Rural Health spokesperson, based in South-West Victoria, said a lack of community, community services and support in rural areas have contributed to a deterioration in health.
The spokesperson said the differences in experiences between rural and urban adults include a greater socio-economic disadvantage (low education and income levels) and structural limitations.
Structural limitations of the rural environment influence the availability of healthy foods, opportunities for physical activity and health promoting services.
[infogram id=”232e1720-dd17-4629-9075-43fca59747d9″]“What we need to focus on is making the healthy choice, the easiest choice. Presently, it often is the hardest choice in rural areas,” they said.
“We need a whole of community approach, by getting community organisations on-board and increasing access and availability to those disadvantaged regionally.”
HESSE Rural Health affirms a need for the Government to invest in preventative healthcare, as critical for the attainment of good health by all.
“Investment in non-hospital services is vital to closing the gap and seeing long-term change, both in health inequity and weight status.”
*Statistics sourced from The Australian Bureau of Statistics, Vic Health and The National Health Performance Authority.
Image source: CLKR.com
